Full of Hot Air (Pneumo) The next big event in my treatment occurred about four weeks into my stay when
my doctor informed me that I was to start receiving pneumothorax treatments (called simply "air" or "pneumo"
by the patients). In this procedure air was introduced between the pleural cavity and the lung in order to partially
collapse the lung and allow it to rest. The doctor explained the procedure while I listened intently, not wanting
to let on that my fellow patients had already described the whole process in vivid detail. 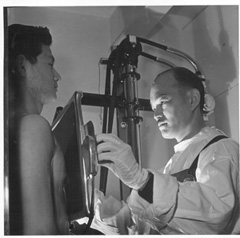
On the big day I found myself in a small room which contained a fluoroscope machine, a padded table
and an apparatus for pumping the air. The fluoroscope machine (shown at right) was a low dosage x-ray which
allowed the operator to see the position of your internal organs before and after receiving the injection of air.
You stood with your back against a big rectangular box apparatus while the operator moved a green phosphorescent viewing
screen up and down your body to view your internal organs and make sure that the pneumo treatment had sufficiently collapsed
the lungs. You might remember back when Buster Brown shoe stores used a small version of a fluoroscope machine to check
out the fit of your new shoes. This concept didn't last too long and was subsequently banned as a health hazard
due to exposing young children to unnecessary radiation.
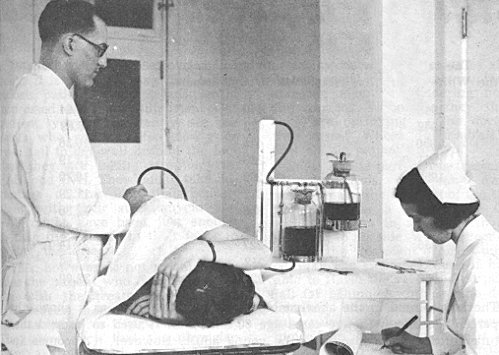 After the initial fluoroscope, I laid on my back on the table. (The
patient in the photo is getting pneumo in his side, another option for collapsing the lung.) The doctor had a needle
which looked very similar to ones used to inflate footballs or basketballs with a threaded head to screw on a pump
hose. But this needle was about an inch longer and had
a sharp tip. My stomach was swabbed with a mercurochrome solution to disinfect the area. Then the needle was inserted
straight down into my stomach area at the belly button level. This was always done without any anesthetic, but surprisingly
there was very little pain involved as the belly skin has a lot of fat and less nerves. Then a long rubber tube would
be screwed onto the end of the needle. The tube was attached to an air pump consisting of two jars of colored liquid,
which you can see in the background of the photo.
 A close-up of the pump is shown at right. When the pump was turned
on, air would flow into the top of the bottle on the right (air in). The pressure would force the colored liquid in
that bottle through a connecting tube into the bottle on the left. As the liquid rose in the left bottle, the
air above it was forced through the tube coming out the top (air out) and into the patient (needle).
The amount the liquid rose in the left bottle was calibrated to determine the amount of cubic centimeters of air you had been
given. The liquid was probably water with color added to aid visibility. The
attending nurse dutifully recorded how many cc's of air you had received. When done, the needle was pulled out and you
were fluoroscoped again to make sure enough air had been inserted to sufficiently collapse the lungs.
The first time receiving pneumo was the worst. It felt like I had a big ball of air
in my stomach (which it actually was!) until you got up and moved around. The air somehow redistributed itself
around the internal organs and felt much better. Occasionally air would "leak" up into the shoulder joints and
be painful for a day or two. I got pneumo once a week for the next 15 months I was at Cresson. After
my discharge, I continued to get pneumo once a week at the Robert Packer Hospital in Sayre, Pa. for another year.
I finally was able to quit pneumo when I started college at the Penn State satellite campus in Hazleton, Pa.
The photo below was sent to me by Dean Knepp of Tyrone, Pa. It gives
a clear description of the purpose and process of pneumo thorax.
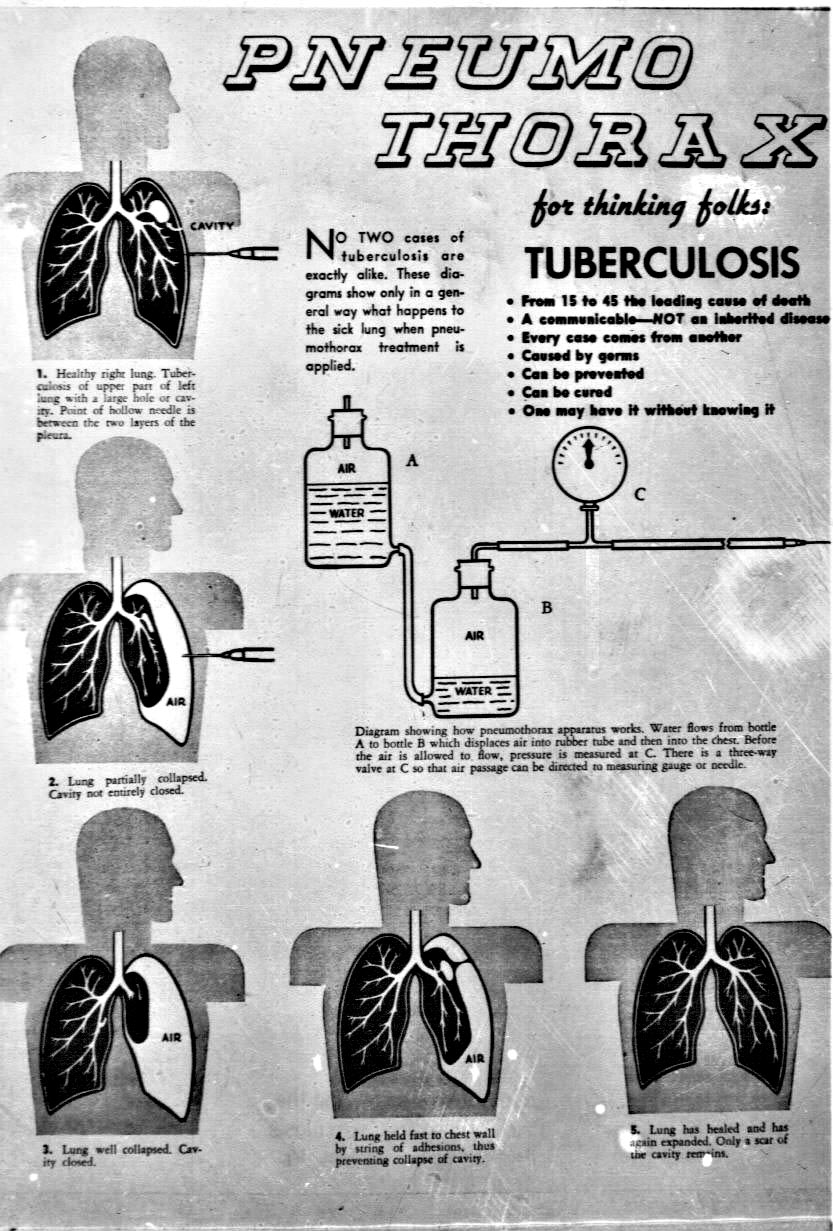

(Photo courtesy of UAMS Library Historical Research Center Digital Collections)
IMPORTANT HEALTH NOTE FOR WOMEN
Pneumo was given to help patients recover from TB. But, unknown at the time, there was
a dangerous side effect. It was not the "air" that was the problem, but the fluoroscopes that were given before and
after each treatment. It was thought at the time that the low dosage x-rays employed in the fluoroscope machine would
have no lasting effects. However, a study published in 1965 showed that women TB patients who had received
pneumo treatments for several years had a much higher rate of breast cancer later in life than the corresponding general
population. A link to the paper discussing these findings is given on the "Favorite Links" page and is entitled "The
Truth About Radiation Dangers". The pertinent part of the report is reproduced as follows:
In 1961, a woman with a rapidly growing breast-cancer came to
his office. He noticed that her cancer had occurred in the upper inner quadrant of her right breast, and that her skin over
the right chest wall, breast, and sternum showed signs of dermatitis (skin inflammation). MacKenzie questioned her carefully about her history, and learned that
she had been treated 14-15 years earlier for pulmonary (lung) tuberculosis. In those years, a common practice was to let one
of the lungs rest, by collapsing it with an injection of air between the chest wall and the lung. This procedure was called
artificial pneumothorax therapy, and in her case, it took place over 46 months. Each time she had a re-fill of air into the
chest, the status of the lung was checked with fluoroscopy, before and usually after.
Fluoroscopy is also called
roentgenoscopy, in honor of Wilhelm Konrad Roentgen, who discovered x-rays in 1895. In roentgenoscopy, examination of a patient
with x-rays takes place while the x-ray beam stays "on," so that the physician can observe what happens when the patient or
the patient's organs are in motion. Roentgenoscopy is thus very different from roentgenography, which is the use of x-rays
to expose a sheet of film (or other types of image-receivers) to produce the usual x-ray picture. Roentgenoscopy, requiring
no development of film, produces information immediately. When
Dr. MacKenzie obtained his patient's sanitarium records, he learned that she had had at least 200 fluoroscopic examinations
during her treatment. The patient remembered that her skin changes began during this period, too. Dr. MacKenzie recognized
that she had radiation dermatitis, and he began to suspect that breast exposure to x-rays might also account for her breast-cancer.
To check on this idea, Dr.
MacKenzie studied almost 800 women who had been treated for tuberculosis in one sanitarium during 1940-1949. The startling
results were published in 1965. Of 510 women who did not receive artificial pneumothorax treatment
and therefore did not have repeated fluoroscopies, one woman had subsequently developed breast-cancer by the time of Dr. MacKenzie's
study. This is a rate of (1 woman / 510 women), or 0.00196. Of 271 women who did receive artificial pneumothorax treatment
with multiple fluoroscopies, 13 had developed breast-cancer by the time of Dr. MacKenzie's study. This is a rate of (13 /
271), or 0.04797. The breast-cancer rate in the irradiated group was (0.04797 / 0.00196), or 24.5 times the rate in the non-irradiated
group. In his paper (p.7), Dr. MacKenzie said:
"From the evidence presented,
it would appear to be a reasonable conclusion that the well-recognized role played by ionizing radiation in the development
of certain other forms of malignant disease can be extended to include carcinoma of the breast in the circumstances presented
by these cases." If pulmonary tuberculosis itself were the cause of the breast-cancers, then the irradiated and non-irradiated
cases should have had similar breast-cancer rates, as Dr. MacKenzie commented. Dr. MacKenzie's finding caused quite a "stir"
in radiation circles.
1965 (March): Ian MacKenzie, "Breast Cancer Following Multiple Fluoroscopies," British Journal of Cancer 1965, Vol.19:
1-8.
|